Can Ebola Really Combat Brain Cancer?
- Published9 Jul 2020
- Author Melissa Mayer
- Source BrainFacts/SfN
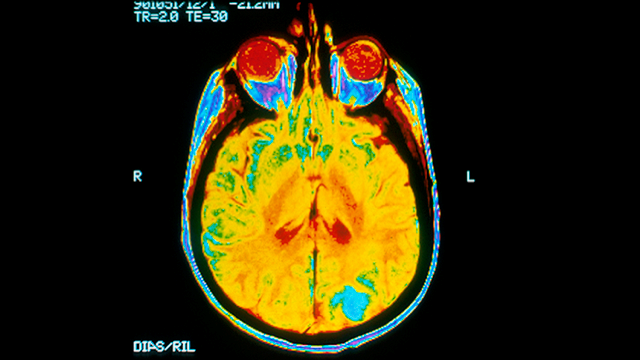
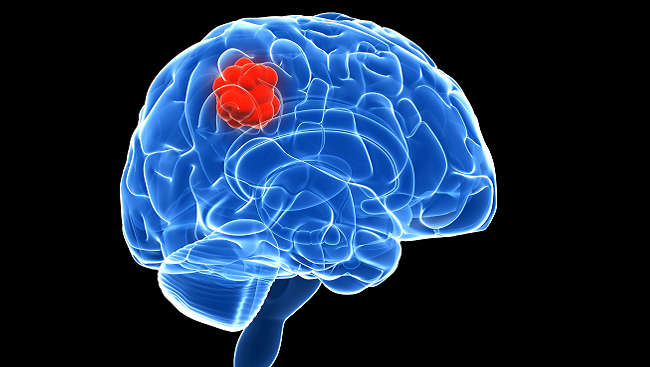
You can tell right away that Margaretta Page is someone you want by your side in a battle against brain cancer. The clinical nurse specialist has been working with brain tumor patients and their families at the UCSF Medical Center for the past 30 years. And she understands well the devastation caused by glioblastoma — the most common and most aggressive form of brain cancer. Patients who receive treatment live about 15 months; those who don’t live around three months.
And during that time, those brain tumors can cause cognitive and emotional changes that Page says affect “the very essence” of a person.
It’s in the face of such devastation that Anthony Van den Pol, professor of neurosurgery at Yale School of Medicine, began looking at extreme solutions — like harnessing a deadly virus that hides from the immune system to target those brain tumors. “[High grade glioblastoma patients] don’t really have a lot of options because surgery, drugs, and radiation all slow the tumor down, but they don’t kill it,” Van den Pol says. “So, there’s got to be something else out there that might work better.”
He thinks that something might be Ebola.
I’m sorry…what?
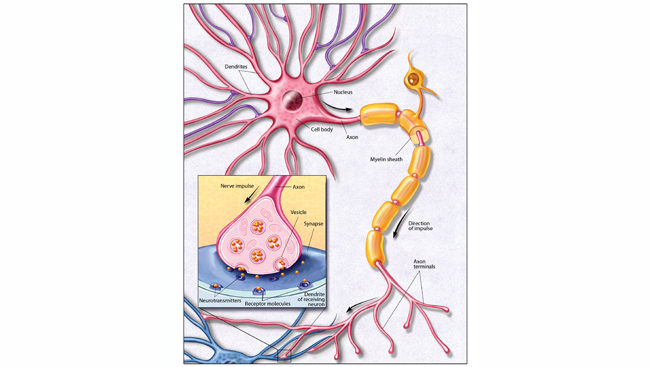
Well, not Ebola Ebola. It’s a hybrid virus originally developed as an Ebola vaccine. It’s made on the skeleton of livestock virus called VSV that can infect and decimate many types of cancer cells. Unfortunately, VSV isn’t particularly effective against brain tumors. Van den Pol’s team seeks to change that by slipping one of Ebola’s seven genes into VSV. The wild type Ebola virus targets and infects liver cells, immune cells, and the lining of blood vessels, but generally not brain cells. So, Van den Pol hoped the combo would work together to target glioblastoma and do so safely.
“It’s been used in a couple hundred thousand people in Africa to protect against Ebola,” explains Van den Pol. “So, even though it sounds very weird, it’s actually safer than VSV on its own.”
It’s so safe that Van den Pol works in a biohazard level 2 lab. That means he follows strict guidelines but doesn’t need the hazmat spacesuits familiar from movies — and the rules are looser than those in place for Ebola or even COVID-19.
A Big Umbrella
Van den Pol’s strategy involves inserting that one Ebola gene into VSV. It codes for a sugar-covered protein that looks a bit like an umbrella. This special area called the MLD sticks out of the virus and shields Ebola from the immune system.
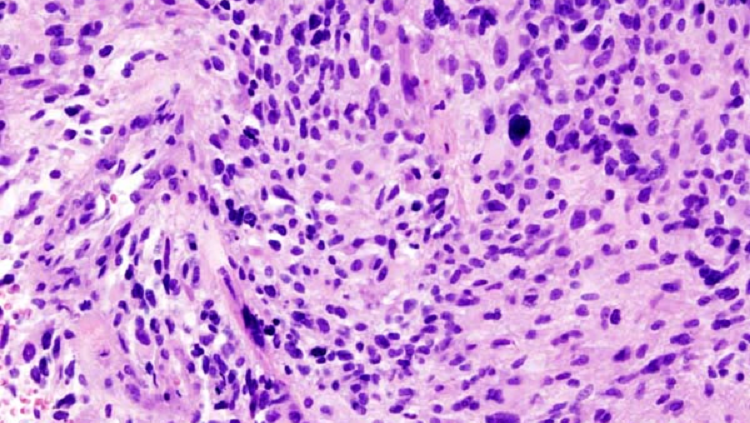
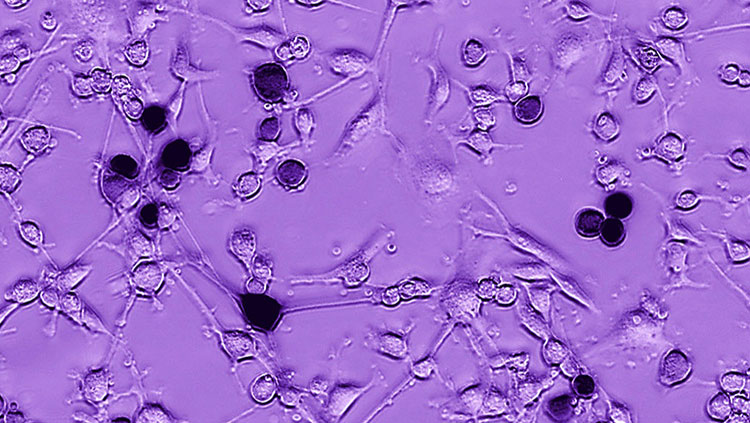
Many tumor cells lack immune defenses to keep viruses out, so presumably the hybrid virus can slip in and begin copying itself. Within a day or two, it should tear the cell open, killing the tumor cell and releasing new viruses.
And that’s exactly what it did when Van den Pol’s team tested the hybrid VSV-MLD in mice. In the study, published in the journal Virology, Van den Pol’s team transplanted human glioblastoma tumors into the brains of mice. The MLD helped the hybrid virus target and kill deadly glioblastoma brain tumors, leaving healthy brain cells uninfected.
Van den Pol thinks the MLD also causes the virus to copy itself more slowly. That gives healthy cells time to mount an immune response while the tumor cells — unable to block the infection — explode. “The virus [triggers] an immune response against the infected cell,” explains Van den Pol. “So, even after the virus has gone, the immune system is still looking around for tumor cells that it associates with this nasty virus.”
Looking Forward
Treating glioblastoma is tricky. “One patient’s tumor may look completely different from another patient’s tumor,” explains Gita Kwatra, CEO of the Glioblastoma Foundation. In fact, this is true for new tumors in the same patient. In the lab, Van den Pol’s hybrid virus destroyed about two-thirds of tumors.
Like any new therapy, this one is years from being ready. Van den Pol must build an extremely pure virus before clinical trials can begin. That said, the existing safety data from the VSV Ebola vaccine gives him a head start.
Page’s patients often participate in clinical trials, and she’s intrigued about this one. “I’ve been in this work a long time, and the needle has moved — but not very far,” Page says. “So, we need a breakthrough. And maybe something like [Ebola] would be the breakthrough.”
And, there is reason for hope. Kwatra points out that discoveries and advocacy took breast cancer survival rates from 20 to 80%. Right now, glioblastoma sits at just 5% “It’s going to take time to really make a difference here — but we’re in it for the long haul,” she says.
In the meantime, Page will be there making sure nobody walks alone: “I know in many cases this disease is not curable. And my job as a nurse is to make that journey easier.”
CONTENT PROVIDED BY
BrainFacts/SfN
References
Home. (n.d.). Glioblastoma Foundation Website. Retrieved from https://glioblastomafoundation.org/
Hathaway, B. (2020, February 12). Scientists find ally in fight against brain tumors: Ebola. Retrieved May 5, 2020, from YaleNews website: https://news.yale.edu/2020/02/12/scientists-find-ally-fight-against-brain-tumors-ebola
Zhang, X., Zhang, T., Davis, J. N., Marzi, A., Marchese, A. M., Robek, M. D., & van den Pol, A. N. (2020). Mucin-Like Domain of Ebola Virus Glycoprotein Enhances Selective Oncolytic Actions against Brain Tumors. Journal of Virology, 94(8), e01967-19. doi: 10.1128/JVI.01967-19