The Race to Understand How COVID-19 Strikes the Nervous System
- Published7 Aug 2020
- Author Lindzi Wessel
- Source BrainFacts/SfN
When the young woman reached the hospital, she was already having trouble speaking and had lost strength in her left arm and leg. Fearing that she might catch the coronavirus, she had delayed heading to New York City’s Mount Sinai Hospital until she could wait no longer. But at the hospital, she learned she already had COVID-19 and that a blockage was stopping oxygen from getting to parts of her brain. She had suffered a devastating stroke. Her doctors labeled it a large vessel occlusion (LVO), a particularly severe form of stroke, which can lead to widespread brain damage — rarely seen in people under 50. She is 33.
“The first thing we noticed that was unusual was a couple of people in their thirties who didn’t have any underlying medical conditions or risk factors for stroke,” says Johanna Fifi, a neuroendovascular surgeon at Mount Sinai, referring to the group of young stroke patients she treated this spring. “Then, we discovered that they were testing positive for COVID.”
Though such cases are considered unusual, doctors at Mount Sinai kept noting other instances like hers as COVID-19 patients flooded their emergency rooms. It’s unusual for doctors at the hospital to see more than one or two young patients with large vessel strokes but from March 23 to April 7, 2020, as COVID-19 swept through New York City, they reported five — all under 50 and all infected by COVID-19. More would soon follow.
Fifi wondered if COVID-19 could be behind the mysterious rise in strokes. She and her colleagues hurried to publish their observations, hoping to warn doctors and the public to be on the alert. “During the height of COVID 53% of our LVO patients were COVID positive,” says Fifi. “Now we are back to pretty much 0%.” Still, she continues to document the cases, unsure if and how the virus caused the devastating symptoms.
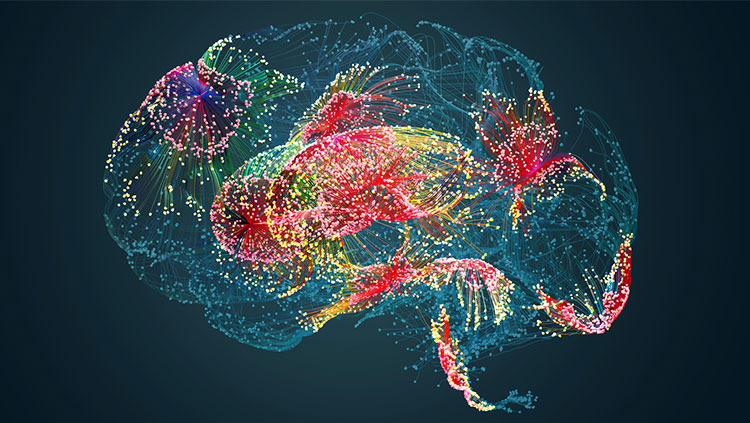
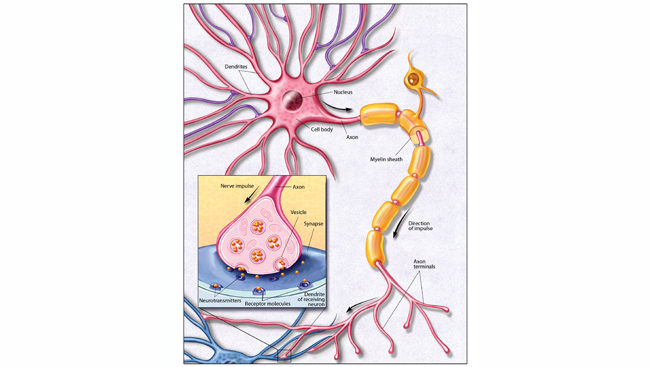
The Mount Sinai strokes are just one in a barrage of complications reported by doctors that might signal nervous system involvement in COVID-19: loss of smell, dizziness, disorientation, and chronic fatigue can persist once the infection is gone. These post-infection effects during recovery are prompting neurologists to call for more attention to how the disease might impact the brain.
In Search of the Virus
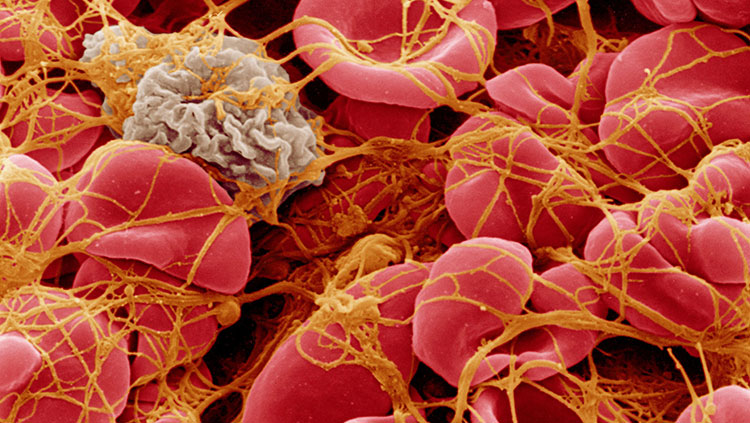
Even if growing suspicions turn out to be right, it leaves the question of how the virus would be doing its damage. Blood clots throughout the body seem to be emerging as a hallmark of the disease. But, in rare cases some viruses, like the virus that causes chickenpox, can target the brain’s blood vessel system and other tissue, wreaking havoc on the brain’s blood supply — but it is not clear that COVID-19 does the same thing.
When it comes to other symptoms, scientists don’t know if they’re caused by COVID-19 directly attacking the nervous system or through indirect effects of damage to other parts of the body.
Respiratory problems from COVID-19 can cause oxygen levels to drop steeply, which is dangerous for the brain. And the out-of-control immune responses, kidney damage, clotting, and other severe symptoms sometimes seen with COVID-19 could easily spell trouble for the nervous system.
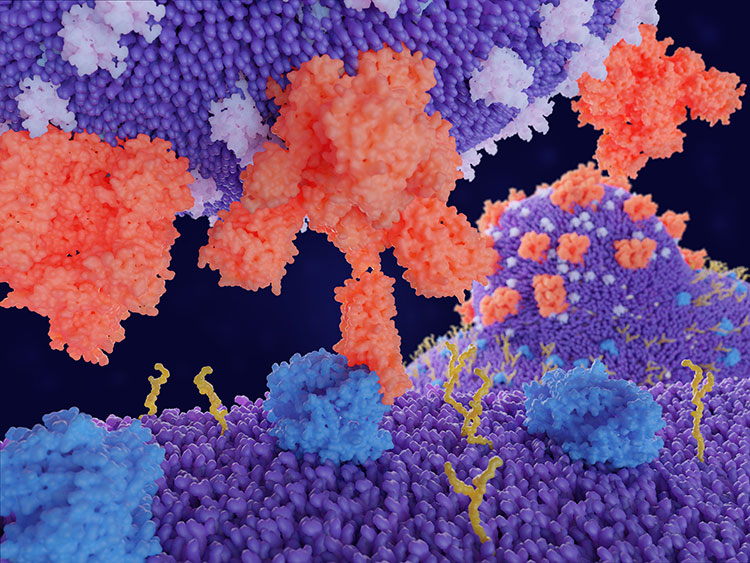
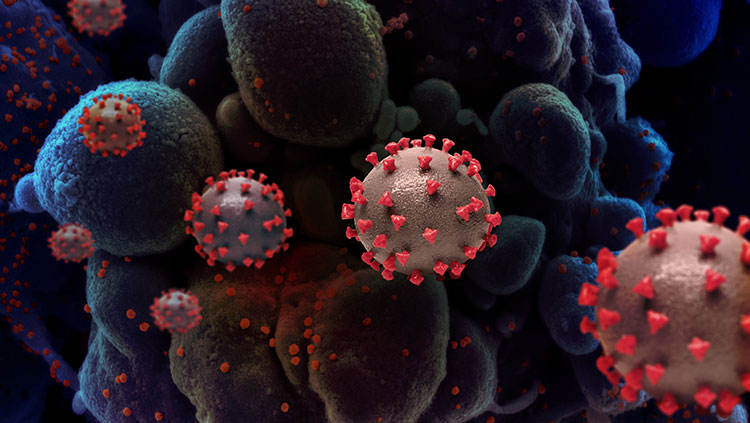
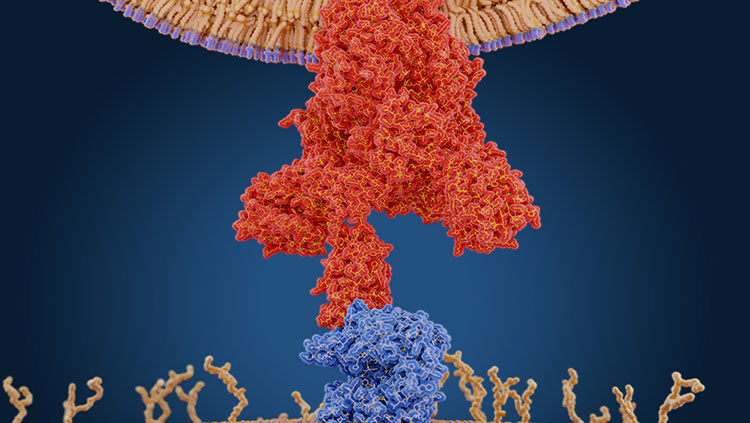
One of the first steps to determining whether the coronavirus might attack the brain directly is to figure out if the virus can even get into the brain, says Michael Wilson, a neurologist at the University of California, San Francisco. He specializes in infectious and autoimmune diseases of the central nervous system. Scientists know that the virus attacks the lungs and other parts of the body by binding to a receptor called ACE2, which it uses to enter cells and begin to replicate itself. ACE2 cells line blood vessels, which carry oxygen throughout the body, including into the brain. But the walls of the brain’s blood vessels are tightly sealed, forming the so-called blood-brain barrier, which typically protects the brain from invading pathogens.
So far, there have only been hints about whether the virus can get into the brain itself. A case report found the virus in the brain of a COVID-19 patient who died, but Wilson, who was not involved in the report, says that it might have come from blood or tissue near the brain after death. Another case study reported evidence of the virus in the cerebrospinal fluid that bathes the brain in one patient, while other studies using spinal taps to search for the virus in the cerebrospinal fluid have turned up nothing.
More research is needed to confirm if and how frequently the virus can reach the brain, Wilson says. And if it can get there, researchers will want to figure out how it does.
Follow Your Nose
While viruses such West Nile virus can get in the brain, the virus only shows up in cerebrospinal fluid at very low levels and only for a short window early in the disease, making it very difficult to detect. Another approach is to test the cerebrospinal fluid for antibodies, which could indicate that the virus was previously present, and that the patient mounted an immune response. But researchers have not yet developed a successful test for COVID-antibodies in cerebrospinal fluid; this is something Wilson and his team are working to solve.
“We just have so many examples of viruses that we know get into the central nervous system, but just don’t hang around for very long,” Wilson says. “Antibody tests are a Plan B way of getting evidence [that the virus has neuroinvasive potential].”
Viruses that cause congestion — including other types of coronaviruses — can also cause temporary smell loss, but, early on, SARS-CoV2 — the virus that causes COVID-19 — perplexed doctors by knocking out smell even in patients without that inflammation and sometimes in people who appeared to have no other symptoms at all. While severe forms of colds can kill olfactory neurons, leading to smell loss that continues beyond the period of heavy inflammation, that doesn’t seem to fit with COVID-19’s pattern either, says Sandeep Robert Datta, a neurobiologist at Harvard Medical School. It takes olfactory neurons months to regenerate once they die, but COVID-19 patients often recover their smell in a matter of weeks although a subset of patients have longer lasting smell loss.

“Those differences are important clues,” Datta says. “Whatever SARS-CoV-2 is doing, it may not be identical to the mechanisms that are used by other related coronaviruses and other viruses that are known to cause the common cold and affect your sense of smell.”
To try and track down the mechanism, Datta’s team has cataloged cell types from smell centers in the nose and brain to see which express ACE2. Cells that lack this receptor shouldn’t be directly vulnerable to the virus. So far, he hasn’t found ACE2 in olfactory neurons themselves, but he has found it in the support cells and vessel system surrounding them, suggesting damage to those cells might be indirectly disrupting the smell signal.
But Datta is also interested in the nose for another reason. The nose is the “doorstep to the brain,” he says. The smell sensitive tissue tucked high up in the nasal cavity directly connects to the brain, and, in the past, scientists have discovered that some viruses can crawl along that pathway to reach the brain itself.
“We know that other viruses can hop from the nose, through the olfactory bulb, into the brain and we know that COVID can cause neurological symptoms,” Datta says. “Is that what’s going on here?”
It will be necessary for researchers to continue documenting cases of neurological symptoms and collect and test tissue from autopsies — a considerable logistical challenge, especially during a pandemic. “This is an area where we just need much more data before we can make any definitive statements,” says S. Andrew Josephson, chair of the department of Neurology at UCSF.
Researchers are just scratching the surface, but they are coming together to tackle the problems COVID-19 presents to the nervous system. It could be many months or longer before we have any solid answers.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Oxley, T. J., Mocco, J., Majidi, S., Kellner, C. P., Shoirah, H., Singh, I. P., … Fifi, J. T. (2020). Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. New England Journal of Medicine, 382(20), e60. doi: 10.1056/NEJMc2009787
Pleasure, S. J., Green, A. J., & Josephson, S. A. (2020). The Spectrum of Neurologic Disease in the Severe Acute Respiratory Syndrome Coronavirus 2 Pandemic Infection: Neurologists Move to the Frontlines. JAMA Neurology, 77(6), 679–680. doi: 10.1001/jamaneurol.2020.1065
Brann, D. H., Tsukahara, T., Weinreb, C., Logan, D. W., & Datta, S. R. (2020). Non-neural expression of SARS-CoV-2 entry genes in the olfactory epithelium suggests mechanisms underlying anosmia in COVID-19 patients. BioRxiv, 2020.03.25.009084. doi: 10.1101/2020.03.25.009084
Sun, L. H., & Sun, L. (2017, November 17). New evidence of brain damage from West Nile virus, scientists say. Washington Post. Retrieved from https://www.washingtonpost.com/news/to-your-health/wp/2017/11/07/new-evidence-of-brain-damage-from-west-nile-virus-scientists-say/
Matacic, C. (2020, June 2). Blood vessel attack could trigger coronavirus’ fatal ‘second phase.’ Retrieved June 30, 2020, from Science | AAAS website: https://www.sciencemag.org/news/2020/06/blood-vessel-attack-could-trigger-coronavirus-fatal-second-phase
Moriguchi, T., Harii, N., Goto, J., Harada, D., Sugawara, H., Takamino, J., … Shimada, S. (2020). A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. International Journal of Infectious Diseases, 94, 55–58. doi: 10.1016/j.ijid.2020.03.062
Zhou, L., Zhang, M., Wang, J., & Gao, J. (2020). Sars-Cov-2: Underestimated damage to nervous system. Travel Medicine and Infectious Disease, 101642. doi: 10.1016/j.tmaid.2020.101642