The Teen Brain, in Flux, Vulnerable to Mental Health Disorders
- Published15 Jun 2020
- Author Agata Boxe
- Source BrainFacts/SfN

A perpetually shy introvert, Deborah Gray often experienced bullying at school. But by 9th grade, things started looking up: bullying had ceased, and Gray finally made friends. But, only on the surface.
Deep inside, a shadow ruled her mind. Constantly down, her self-esteem waned. Convinced she would fail at whatever she tried, she spent most days in her room.
“I felt like I was in a fog,” says Gray, now a 56-year old event coordinator in the San Francisco Bay Area. “I was just kind of stumbling around in the dark, trying to find a way out.”
Many teens, like Gray in her youth, suffer from depression. Research suggests teenagers are particularly vulnerable to depression, anxiety, and, according to some data — obsessive-compulsive disorder (OCD). The reasons behind these susceptibilities may lie in the complex stew of neurodevelopmental, hormonal, and social factors.
Remodeling During A Storm
The teenage brain undergoes dynamic remodeling and rewiring. “There is a lot of maturational change that is occurring in the brain during this time period,” says Carrie Bearden, a professor of psychiatry and behavioral sciences and psychology at the University of California, Los Angeles. “That makes it both a period of what we think of as a lot of opportunity, but also a lot of vulnerability for things to go wrong.”
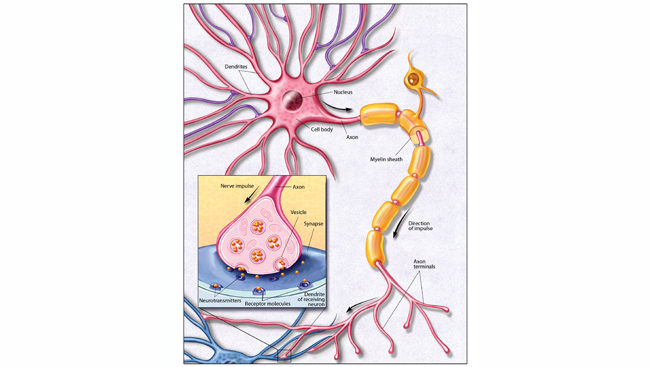
One major change — which occurs partly due to hormonal fluctuations during adolescence — is the transition from creating new synapses to pruning unneeded ones, helping the brain to become more specialized, says Deanna Barch, chair and professor of psychological and brain sciences at Washington University in St. Louis. Moreover, brain regions involved in emotional reactivity and reward, such as the amygdala and nucleus accumbens, mature faster than the prefrontal cortex, which governs thinking and decision making. “Particularly, delayed integration and coordination of prefrontal functions with those reward-sensitive regions is related to the vulnerability and the way in which things might go awry during this time period,” Bearden says.
In 2017, about 3.2 million adolescents in the United States experienced at least one major depressive episode — a period of at least two weeks when they felt depressed or lost interest in daily activities and experienced symptoms like problems with sleep or concentration, according to the National Institute of Mental Health. Barch says depression rates rise with puberty compared with childhood and continue to stay elevated in adulthood. “Whatever causes them to increase seems to be sustained, but we don’t know what that is specifically,” she says.
Research points to teenage bullying as a contributing factor to depression and related disorders, both in teens and adults. As young people begin to place more value on peer relationships in their teens, trauma from the painful experiences can become a signature of their brains.
A Bundle of Nerves
Jemila Jackson struggled with anxiety since childhood, but when she was about 15 years old her constant worrying morphed into panic attacks. Her breathing would become very rapid, and she would start feeling like she was suffocating. She remembers experiencing one of these attacks on the subway. “All of a sudden, I just felt so panicky I had to leave the subway car,"says Jackson, now a 34-year-old transformation director of I’m Still Standing, a women’s Christian ministry.
Less than 2% percent of children ages three to five are diagnosed with anxiety disorders, but its rates increase to more than 6% for ages six to 11 and more than 10% for ages 12 to 17, according to data from the Centers for Disease Control and Prevention.
All of a sudden, I just felt so panicky I had to leave the subway car
To this end, researchers are focusing on the connections between the prefrontal cortex and the amygdala — the almond-shaped structure that not only processes emotions but also detects and responds to threat, says Dylan Gee, an assistant professor of psychology at Yale University. The prefrontal cortex, which regulates fear and other emotions and controls amygdala activity, continues to mature and change well into adulthood and so do its connections with the amygdala.
“Evidence suggests that the regions that are most involved in emotional processing and regulation are particularly in flux during adolescence,” Gee says. Issues with emotion regulation have, in turn, been implicated in both anxiety and depression. Examples include tendencies to ruminate, or think obsessively about a problem, as well as to hide how a person really feels by modifying their facial expressions. People who have problems regulating their emotions are also less likely to mentally reframe negative events or challenges in a way that present solutions or reveal to others what’s troubling them.
Treating the Signs at the Start
Morgan Rondinelli has been a perfectionist since she was a child. She also remembers being inundated with intrusive thoughts as early as in kindergarten. She would worry that something bad would happen to her family, leading her to “knock on wood to make it not happen.” In high school, her perfectionism started to spiral out of control. She studied constantly, obsessed with getting straight As. In college, she began doubting her ability to comprehend material, so she would spend a lot of time reading it over and over. “I was just constantly studying and afraid that I would forget information, and afraid that I would start a fire, and hoarding things,” she says. She did not get better until she received treatment following an OCD diagnosis at 19. Rondinelli mentioned that she received exposure and response prevention (ERP) for OCD. ERP is the evidence-based treatment for OCD, sometimes in combination with medication and other therapies.
I was just constantly studying and afraid that I would forget information, and afraid that I would start a fire, and hoarding things
Teenage years may also be a prime time for the onset of obsessive-compulsive disorder. In recent years, scientists have looked at the mechanisms of OCD in young people, concluding that kids with perfectionistic tendencies are more likely than other children to developed OCD as teens. For example, when researchers asked study participants to draw perfect circles, children with such tendencies became overly critical of their work after receiving negative feedback from evaluators.
For teenagers with depression and anxiety disorders, early diagnosis and detection are key. Treatments range from medications to cognitive behavioral therapy, which aims to modify the negative patterns of thinking and dealing with emotions at the root of the problems.
Gray and Jackson eventually found relief for their symptoms later in life — Gray through medication and Jackson through her faith, counseling, and mentorship — and are feeling much better these days. “I have very good self-esteem,” says Gray. “I have very strong sense of self.”
CONTENT PROVIDED BY
BrainFacts/SfN
Discussion Questions
1) What is happening to the brain during adolescence that exposes risk to teen emotional and mental health?
2) What brain areas may be at the root of teen susceptibility to depression and anxiety-related disorders?
3) How might bullying play a role in depression and anxiety during childhood and adolescence?
References
Bowes, L., Joinson, C., Wolke, D., & Lewis, G. (2015). Peer victimisation during adolescence and its impact on depression in early adulthood: Prospective cohort study in the United Kingdom. BMJ : British Medical Journal, 350, h2469. doi: 10.1136/bmj.h2469
Cisler, J. M., & Olatunji, B. O. (2012). Emotion regulation and anxiety disorders. Current psychiatry reports, 14(3), 182–187. doi:10.1007/s11920-012-0262-2
Data and Statistics on Children's Mental Health, CDC. https://www.cdc.gov/childrensmentalhealth/data.html
Dryden, J. Perfectionism in young children may indicate OCD risk. https://medicine.wustl.edu/news/perfectionism-in-young-children-may-indicate-ocd-risk/
Joormann, J., & Gotlib, I. H. (2010). Emotion regulation in depression: relation to cognitive inhibition. Cognition & emotion, 24(2), 281–298. doi:10.1080/02699930903407948
Kaltiala-Heino, R., & Fröjd, S. (2011). Correlation between bullying and clinical depression in adolescent patients. Adolescent health, medicine and therapeutics, 2, 37–44. doi:10.2147/AHMT.S11554