Alzheimer's Disease: A Tale of Two Proteins
- Published19 Oct 2021
- Source BrainFacts/SfN
A hallmark of Alzheimer’s disease is atrophy of the brain. Scientists have attributed this to dysfunction of two proteins: beta-amyloid and tau.
This is a video from the 2021 Brain Awareness Video Contest.
Created by Veda Dayananda.
CONTENT PROVIDED BY
BrainFacts/SfN
Transcript
Fifty-one-year-old Auguste Deter suffered from severe and mysterious mental symptoms. Her memory was rapidly deteriorating. She had auditory hallucinations and delusions that people were out to kill her. Her own home became an endless, puzzling maze, and at times she was delirious, screaming loudly in the middle of the night.
Deter passed away in 1906. An examination of her brain revealed severe atrophy, or shrinkage. When stained and then viewed under the microscope, her brain was found to be riddled with abnormal clumps of proteins. The neuroscientist who performed this autopsy was Dr. Alois Alzheimer, and what he had observed in Deter was Alzheimer's disease.
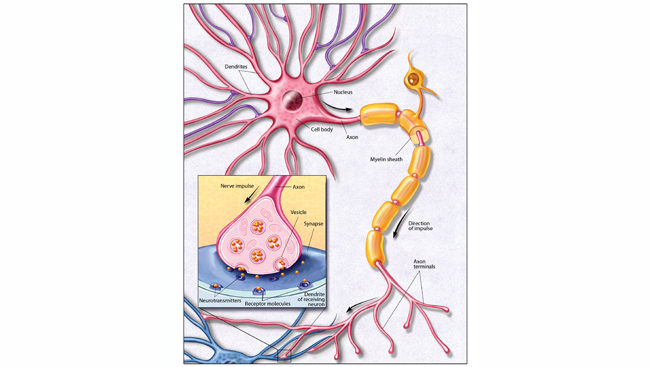
There is still a lot to uncover, but neuroscience has come a long way since Alzheimer's time. We now know that these abnormal proteins viewed under the microscope were beta-amyloid and tau, the two suspected culprits behind Alzheimer's disease. Alzheimer's is one of many neurodegenerative diseases, which involve a progressive degeneration and death of neurons. Almost all neurodegenerative diseases involve a buildup of abnormally shaped proteins called prions. These proteins lose their characteristic three-dimensional shape and this prevents normal functioning.
When we think of Alzheimer's we often think of a certain age group, but it's important to note that aging is not synonymous with Alzheimer's and other forms of dementia. While Alzheimer's risk does increase with age, rare forms of the disease can affect individuals as young as 30 years old. The normal changes that we see with aging are actually quite subtle and mainly affect the speed of thinking and the control over attention. Alzheimer's Disease, on the other hand, has a whole host of symptoms as we saw with Deter — memory loss, disorientation in time and place, changes in personality and behavior, among others.
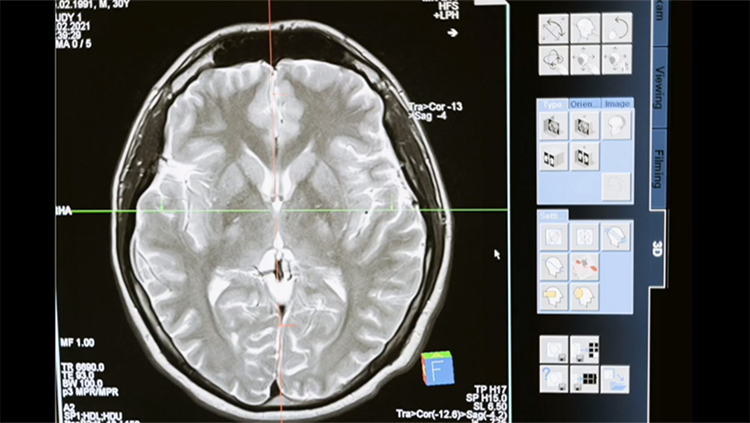
But, what actually happens in the brain? If we look at a side-by-side comparison of a diseased brain and a normal one, we notice a startling difference in the thickness of the cerebral cortex, the outermost layer of the brain. This is due to neurons and their connections breaking down. The hippocampus, involved in the storage of long-term memories, shrivels. Damage to the hippocampus affects an individual's episodic memory, which is the memory of our everyday events. Semantic memory, our repository of facts and data, is preserved until the later stages of the disease.
Additionally, neurons in a region of the brain called the nucleus basalis of Meynert degenerate. These neurons produce a chemical messenger called acetylcholine which plays a role in movement, memory, learning, and more. In Alzheimer's patients, acetylcholine levels are low. Therefore, common treatments for Alzheimer's are medications that increase acetylcholine levels. To compensate for the shrinkage of the cortex and hippocampus, cavities in the brain known as the ventricles enlarge.
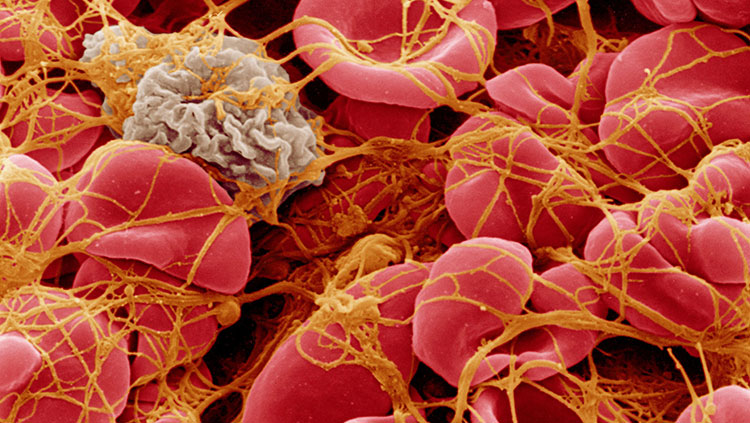
But, what causes the neurons to break down in the first place? Researchers suspect that two proteins — beta-amyloid and tau — are the main culprits of Alzheimer's disease. Beta-amyloid is a sticky protein that tends to clump outside of neurons. Beta-amyloid is derived from the amyloid precursor protein, or APP. Proteolytic enzymes called secretases cleave the APP protein to form beta-amyloid, which then aggregates extracellularly to form large plaques. These plaques bind to receptors and initiate erosion of the synapse, the special zone of contact between neurons. This hinders communication in the brain.
Neurons contain a network of fibers that carry substances from one part of the neuron to another, kind of like a highway. The tau protein normally functions as a microtubule-associated protein, where it stabilizes the elements that make up this fibrous network. In Alzheimer's, tau aggregates to form tangles inside of neurons. Tau proteins become hyperphosphorylated and highly insoluble, causing them to build up inside neurons. When dysfunctional, tau can damage cellular transport by blocking the neuron's fibrous tracts. Eventually, the neuron completely degenerates.
The cellular changes that we see with plaques and tangles can first appear a decade before the onset of symptoms. Normally, special cells in the brain called astrocytes help to clear out beta-amyloid. In a diseased brain, astrocytes switch from a protective role to one that promotes beta-amyloid accumulation and plaque formation.
Research into Alzheimer's disease and neurodegeneration altogether is an exciting field. Scientists at MIT are exploring the possibility of gene editing technology called CRISPRoff that has the potential to reduce the expression of the gene that codes for the tau protein. Research in this field has a long way to go, and there are still a lot of questions that are unanswered. For example, is beta-amyloid a cause or consequence of Alzheimer's? Does susceptibility depend more on genetics or environment? Could we possibly find a cure for neurodegenerative diseases?
Science is making great achievements, but it can only take us so far. Unfortunately, Alzheimer's is an irreversible and progressive disorder, and currently there is no cure. We need to promote love and compassion for individuals afflicted with Alzheimer's and any other neurodegenerative disease.