Cognitive Behavioral Therapy (CBT) and Transcranial Magnetic Stimulation (TMS): What Are These Therapies and How Are They Used?
- Published7 Feb 2018
- Reviewed7 Feb 2018
- Author Melissa Galinato
- Source BrainFacts/SfN

When you have a cold, you might have a runny nose, a headache, and a cough. You may take different medications to treat each symptom to soothe your throat or ease your sneezing. Like treating a cold with multiple symptoms, there are different types of therapies to treat the multiple symptoms of depressive disorder, widely known as depression. Cognitive Behavioral Therapy (CBT) and Transcranial Magnetic Stimulation (TMS) are two therapy types that address specific symptoms of depression.
More than 300 million people around the world have depression, which is a common mental illness with multiple symptoms such as persistent sadness, irritability, a feeling of worthlessness, and loss of interest in activities—especially in things that previously brought joy or excitement.
With Cognitive Behavioral Therapy (CBT), a therapist helps a patient with depression to focus on understanding how three things - thoughts, feelings, and behavior - affect each other. “The goal of CBT for depression is to start targeting problematic thoughts and actions that are occurring in the present – as opposed to looking back in the past for a cause – teaching patients skills that they can use to become more aware of their negative thoughts, evaluate their validity and, when not accurate, replace them with more realistic/balanced ways of thinking,” says Simon Rego, Chief Psychologist at Montefiore Medical Center/Albert Einstein College of Medicine in New York.
“At the same time, the other goal of CBT is to help patients change maladaptive patterns of behavior, gradually increasing activities of pleasure and accomplishment, which are known to enhance mood. Taken together, changing how you think and what you do can have a powerful positive impact on your mood.”
Imagine setting a goal - like running a marathon for the first time. A running coach could help you reach that goal by giving you tips and developing a training to slowly build up your strength. In CBT, the therapist acts like a coach and helps people identify goals such as driving a car or giving a speech. Then the therapist helps to figure out actions to reach those goals such as practicing thinking strategies, writing in journals, and doing homework assignments between appointments. Doing these activities in CBT can help people learn coping skills, build self-confidence, and have a sense of control, and a growing number of studies show that CBT works very well for treating depression and several other mental health conditions.
“CBT is an effective treatment for depression because it targets the two main areas where people with depression struggle: negative thoughts and unhelpful behaviors,” said Rego. “The main theory in CBT is that how we feel is directly influenced by how we think and what we do (or don’t do). In the case of depression, we know that people tend to have many negative thoughts about themselves, the world, and the future (e.g., I am a failure, I’ll never get better, no one cares about me, I don’t have the energy to do anything, etc.) which only serve to perpetuate their negative mood.”
Another therapy called Transcranial Magnetic Stimulation (TMS) can be used for some patients with depression who do not get better with antidepressant medications or other treatments. “In our experience, TMS is an appropriate treatment for major depressive disorder, moderate in severity and who are still functioning in the home, community, and who have failed multiple antidepressant medications,” said Ananda Pandurangi, medical director and chair of inpatient psychiatry in the Department of Psychiatry at Virginia Commonwealth University School of Medicine. “It is not appropriate for patients with either “mild” depression or those with severe depression including those with psychosis or catatonia,” said Pandurangi, noting that psychotherapy and medications may be more appropriate for patients with mild to severe depression.
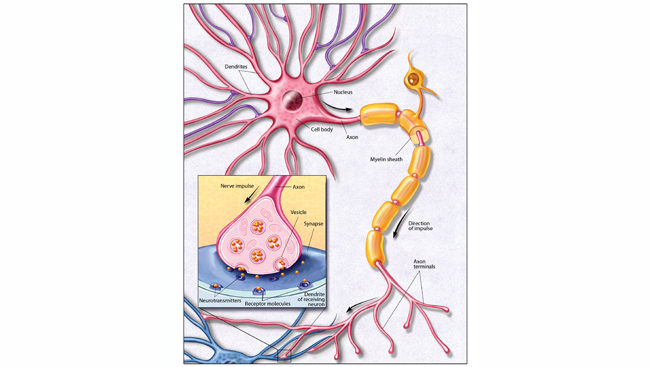
TMS aims to alter brain circuitry. Using an electromagnetic coil, called a stimulator, to affect brain activity and treat depression, TMS treatment involves a doctor placing the stimulator near the forehead against the scalp. This activates brain cells in an area of the brain that includes the prefrontal cortex and controls mood and depression.
Sessions typically use repetitive TMS (rTMS) where recurrent magnetic pulses stimulate the brain. In 2008, the FDA approved rTMS for depression treatment after several research studies showed this TMS treatment lowers signs of depression and improves mood in people with treatment-resistant depression.
CONTENT PROVIDED BY
BrainFacts/SfN