Can Brain Science Help Promote Good Health?
- Published14 Apr 2015
- Reviewed14 Apr 2015
- Source The Dana Foundation
Better health habits can save more lives than the flashiest treatment breakthrough. According the National Institutes of Health, 40% of premature deaths in the US can be attributed to preventable behaviors like smoking, poor diet, and inactivity
But it's hard to get people to change their ways. Smoking still causes nearly a half-million deaths yearly in the US, and 60-85% of the world’s population lead sedentary lives, increasing their risk of heart disease, stroke, diabetes, and certain cancers.
Can brain science help? In recent years researchers have been using techniques like neuroimaging to identify persuasive strategies such as public service ads (PSAs) that effectively improve health behavior, explore why they work, and suggest how they might work better.
Those in the field see enormous promise. “I believe this has the potential to greatly change the landscape of how we evaluate health messages and provide a fantastic tool to optimize their design,” says René Weber, director of the Media Neuroscience Lab at University of California, Santa Barbara.
The tell-tale brain
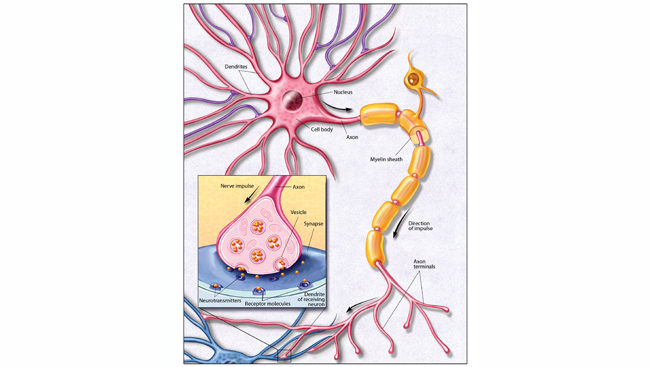
For several years, Emily Falk of the Annenberg School of Communication at University of Pennsylvania has done pioneering work using brain imaging to predict the success of health-promoting communication. In a 2011 fMRI study, her research team showed smokers ads designed to help them stop, and found that activity in the medial prefrontal cortex (MPFC) region of the brain while viewing the ads was associated with successful quitting a month later.
A paper for which she was lead author the following year put neuroimaging to the test in a “neural focus group”: the researchers showed 31 smokers three ad campaigns promoting a smokers’ quit phoneline, and found that MPFC activity predicted which would work in the real world—more accurately than the smokers’ subjective ratings of the campaigns' effectiveness (or those of industry experts).
“This is not to say that brain imaging is better than self-report,” Falk says. “It’s complementary; it gives us information that people don’t have access to.”
Now Falk has gone a step further. In an fMRI study published in PNAS this year, her research team documented how an intervention to improve health (reduce sedentary behavior, here) influenced brain function, and linked this change to ots effectiveness.
In the study, 45 participants heard messages detailing the risks of being sedentary, and advice for getting active. For half, the messages were preceded by “self-affirmation” messages encouraging them to reflect on what was important to them, like family or creativity.
“People don’t like to be criticized, to be told what they do is harmful or destructive. They feel defensive,” Falk says. By bolstering their sense of self-worth, affirmations could make them more open to good counsel. Indeed, earlier studies have shown self-affirmation an effective adjunct to health promotion.
It worked here too. Physical activity increased significantly more in the self-affirmation group over the following month, compared to controls.
The brain findings were also familiar: Greater MPFC activity while participants viewed the messages predicted improvements in sedentary behavior.
“I think this paper adds to our understanding of how affirmation works and how the brain might predict health behavior change,” Falk says: the MPFC is involved in self-reflection and evaluation; it may be that health messages are effective when seen as valuable to oneself, and that affirmations increase this sense of value.
Beyond earlier research that simply correlated MPFC responsiveness and outcome, the study “shows that you can systematically manipulate this area with an intervention that increases its activity,” she said.
“Emily’s paper did a nice job arguing the value of neuroimaging,” says Elliot Berkman, director of the social and affective neuroscience lab at University of Oregon. “There’s a clue about self-affirmation that we wouldn’t have if we just had behavioral results and didn’t look in the brain.”
The findings suggest additional interventions worth exploring, says Berkman, who has collaborated with Falk on other projects but was not involved in this study. “The same region is sensitive when we value what friends, peers, and family think. To strengthen this [effect] we might bring in a social aspect, like encouraging messages from friends and family.”
Powerful pictures
Neuroscience has also weighed in on a particularly contentious form of health communication: graphic warning labels (GWLs) on cigarette packs, which add images to texts warning of health risks and are standard in Canada and Europe but not the US.
Congress authorized GWLs in 2009. But tobacco companies challenged the emotionally powerful images chosen by the FDA (e.g. a diseased lung, a cadaver, a man blowing smoke through a tracheotomy opening), claiming they simply scare consumers away from a legal product, not educate them about its dangers.
The courts have thus far agreed, saying the evidence that labels must frighten to communicate effectively isn’t compelling enough to justify abridgement of the companies’ first amendment rights.
“Research [on GWL effects] has been based on self-report measures, such as intention to quit, which aren't terribly reliable, and population studies like changes in smoking patterns after labels are introduced,” says Daniel Langleben, of University of Pennsylvania. “Biological research would be more objective—it can bypass the conscious mind to how people really feel and think.”
The basic question, he says, is whether strongly emotional labels accomplish key goals—promoting learning, for example—better than tamer pictures.
In an fMRI study published in Tobacco Control this year, Langleben and An-Li Wang showed that people remembered high impact labels better and reported less urge to smoke.
There were biological differences too: emotionally potent labels aroused more activation in the amygdala, hippocampus, and inferior frontal gyri, “areas that facilitate memory processing, especially during the encoding period,” says Wang, also of the university. “This may indicate better consolidation and long-term effect: the next time you see a cigarette pack it would trigger the memory.”
In another study, the researchers used EEG to assess GWLs’ effect on craving. The smokers reported less craving when shown smoking cues (like a picture of a lit cigarette), after viewing both more and less emotional GWLs. But EEG showed that only the powerful labels damped down the brain’s electrophysiological response to cues.
Although subjects said less emotional images also made them want to smoke less, “the brain told us they’re still paying a lot of attention to smoking cues,” Wang says.
“This is clearly important work,” says Berkman. It presents “good hard evidence that GWLs reduce craving.” The public health relevance of the neurophysiological findings, on the other hand, “is less clear. It’s time to start evaluating: does this actually help people stop smoking?”
Such testing is in the works, says Langleben. The findings he and Wang reported “were preliminary… they mapped out brain responses to more and less emotionally powerful images.” In a study now in progress, the researchers will measure urinary cotinine, a marker of nicotine use, after a month of GWL exposure. “Whether it is reduced more in the scary label group will be very important data,” he said.
Marketing health
With gathering evidence that neuroscience can help predict communication effectiveness , Langleben proposes an expanded role in crafting health messages by tracking brain responses.
“Let us in on the ground floor with these techniques, to see if we can design better labels,” he says.
René Weber envisions a collaboration between neuroscientists and communication scholars that might “dissect and analyze health messages, moment by moment, to identify the pieces of information that trigger value processing or increased attention… and help us understand how to optimize them.”
Cognitive styles differ among individuals, as do attitudes and beliefs that make some resistant to healthy behavior change. Neuroscience research, he conjectures, could help tailor interventions to the unique neurological makeup of high-risk people.
But his optimism comes with caveats. Weber points to neuromarketing—which uses science to sell merchandise, not health—as a cautionary tale. Until recently, he says, the field was dominated by “a lot of poor research..there's a “buy button” in the brain that if activated will make you choose a brand. Real rubbish.”
A thoughtful approach that avoids simplistically equating brain activation with particular emotions or motives is essential to keep health communication research on the right path, he says.
And ethical questions can’t be ignored. Inducing healthier behavior would seem an irreproachable goal, “but if you think about persuading people with strong attitudes to change them, it could have a dangerous component,” Weber says. “From our perspective, the best you can do is give your knowledge free to the world, so everyone can use it.”
- By Carl Sherman
CONTENT PROVIDED BY
The Dana Foundation is a private philanthropic organization that supports brain research through grants and educates the public about the successes and potential of brain research.