Neurological Trauma
- Published1 Apr 2012
- Reviewed1 Apr 2012
- Source BrainFacts/SfN
Brain injury is all too common, but treatments are being improved constantly. Traumatic brain and spinal cord injuries can lead to significant disabilities and death. In the United States, an estimated 1.7 million people suffer traumatic head injuries each year, and roughly 52,000 will die. The leading causes of traumatic brain injury are falls and motor-vehicle related events.
Those who survive a brain injury face a lifetime of disability, with economic costs approaching $60 billion annually. An estimated 265,000 individuals in the United States are living with spinal cord injury. Each year, about 12,000 new injuries are reported, caused mostly by motor vehicle accidents, sports injuries, violence, and falls. The cost of caring for these individuals approaches $10 billion a year. Such facts point to the pressing need to advance our understanding of these injuries, with the goal of developing strategies to support long-term recovery.
No magic bullet has yet been found, but doctors have discovered methods to stave off severe neurological damage caused by head and spinal cord injuries and to improve neurological function. This is accomplished by working to prevent secondary pathogenesis, or damage that occurs after the initial insult; support regeneration and repair; and refine and optimize rehabilitation techniques.
Traumatic Brain Injury
Greater access to and use of CT and MRI offer physicians the opportunity to diagnose the extent of tissue damage and determine medical management. In general, patients who arrive in the emergency room and are diagnosed with a severe head injury are monitored for pressure on the brain from bleeding or swelling. Treatments for increased intracranial pressure include the removal of cerebrospinal fluid, moderate hyperventilation to temporarily decrease blood volume, and the administration of drugs to reduce cellular metabolism or to remove water from the injured tissue.
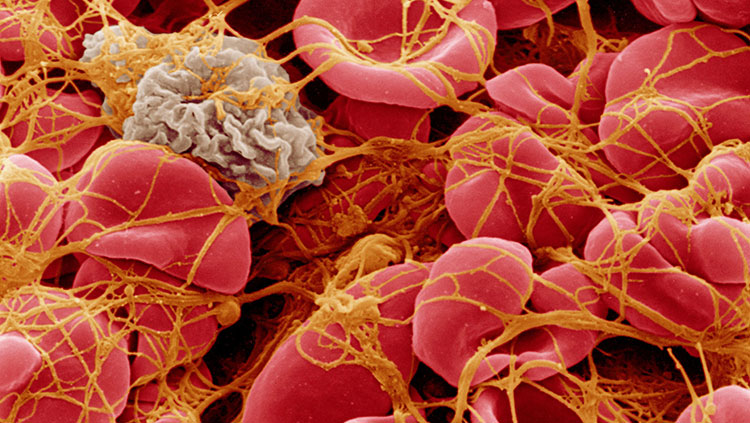
In addition to helping the physician avoid cerebral edema, or swelling as a result of excess accumulation of water in the brain, and reductions in cerebral blood flow following traumatic brain injury, imaging can reveal lesions produced by the initial injury. These lesions can consist of bleeding on the surface or within the brain as well as the formation of contusions, or bruises. Once blood leaks from vessels and comes into direct contact with brain tissue, it causes localized pressure, reducing cerebral blood flow. The blood itself also can be toxic to brain cells. Contusions can be troubling because they can increase pressure as well as contribute to the development of post-traumatic epilepsy. As a last resort to reduce increased intracranial pressure, part of the skull may be removed to allow the brain to swell, a procedure known as a decompressive craniectomy.
No drug for improving outcomes of traumatic brain injury has yet been approved. A recent pilot clinical trial for patients with moderate to severe closed-head injury found that the hormone progesterone cut the number of deaths in severely injured patients by 50 percent. Those in the moderately injured group had improved functional recovery 30 days after injury. Treatments for the injury-induced reduction of cerebral blood flow include the administration of drugs that increase mean arterial blood pressure. In combination with the reduction of intracranial pressure, this treatment results in an increase in blood flow, allowing more blood to reach vital areas.
Spinal Cord Injury
Methylprednisolone is the only FDA-approved treatment for spinal cord injury. While there is increasing controversy about the use of this steroid, earlier studies showed efficacy when people with spinal cord injuries received high intravenous doses within eight hours of the injury. Building on these clues and insights into precisely how and why spinal cord cells die after injury, researchers hope to develop new therapies to reduce the extent of spinal cord damage after trauma. In that context, there is a growing interest in early intervention of the inflammatory response to prevent secondary damage by this response and support neurologic recovery.
Scientists have known that, after a spinal cord injury, animals can regain the ability to bear their weight and walk at various speeds on a treadmill belt. More recently, scientists have recognized that the level of this recovery depends to a large degree on whether these tasks are practiced — that is, trained for — after injury. People with spinal cord injury also respond to training interventions.
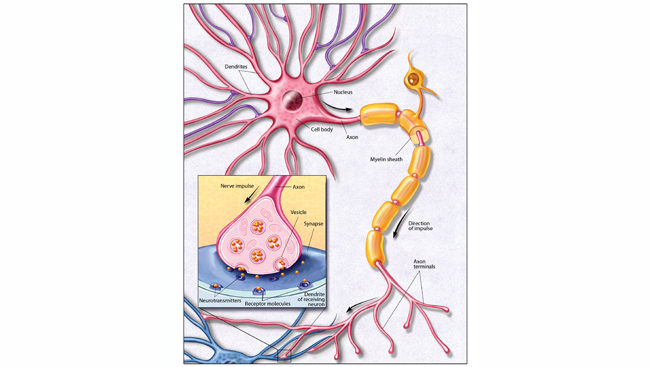
Scientists have also discovered that new nerve cells can be born in the adult brain, but these new cells do not seem sufficient to help the injured brain regenerate. Studies are underway to determine how to jump-start the pathway that stimulates neurogenesis, the birth of new nerve cells. Researchers are trying to decipher how certain environmental cues can be used or overcome to attract these new cells — or transplanted stem or progenitor cells — to areas of brain injury to facilitate regeneration and repair.
These and other recent discoveries are pointing the way toward new therapies to prevent secondary damage and promote nerve regeneration after brain and spinal cord injury. Although these new therapies have not yet reached the clinic, several of them are on the path to clinical trials.
CONTENT PROVIDED BY
BrainFacts/SfN