Migraines: What's Light Got to Do With it?
- Published26 Jul 2019
- Author Vandana Suresh
- Source BrainFacts/SfN

For 37-year-old mother and hairstylist Amy Barger, migraine headaches usually go hand in hand with debilitating light sensitivity. “Light makes my headache worse, puts me in a bad mood, and gives me nausea,” she says. “I can’t concentrate, so I can’t work.”
For 80 percent of people with migraines, light both triggers and exacerbates their headache pain says Andrew Russo, professor of molecular physiology and biophysics and neurology at the University of Iowa.
In teasing apart how, scientists are delving into both the nerve connections between the eye and the brain and the underlying biology of inflammation.
The idea that light interacts with migraine pathways in the brain to cause light sensitivity, or photophobia, isn’t intuitive. “It’s difficult to explain how light can induce pain in the head or in the eye,” says Rodrigo Noseda, assistant professor of anesthesia at Harvard Medical School.
Noseda and colleagues took an initial step in understanding this mystery when they studied why some blind people with migraines get photophobia. Even though they couldn’t see, this group of blind migraineurs possessed intact connections between the retina and brain. In other words, they could discern whether a room was illuminated, but they could not discern shapes or color. These observations lent a valuable insight — light detected in the eyes, but not necessarily seen, can cause photophobia.
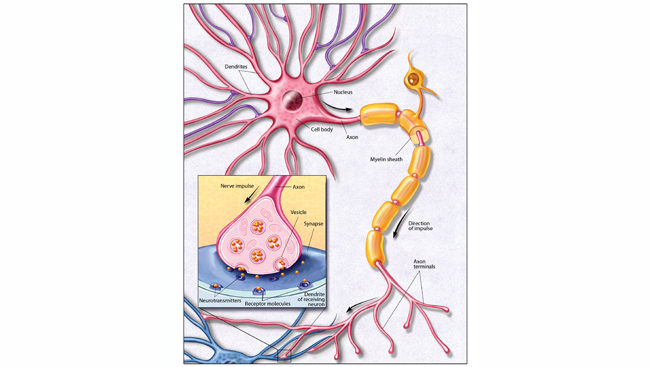
The finding pointed to a role for cells known as intrinsically photosensitive retinal ganglion cells (ipRGCs). They detect light but don’t contribute to sight. Like retinal rods and cones, ipRGCs produce their own light-sensitive protein called melanopsin, which is more sensitive to blue light. Unlike rods and cones needed to see, ipRGCs instead coordinate involuntary functions such as circadian rhythms and pupillary light reflex (PLR) when eyes are illuminated. Because most people with migraines find blue light uncomfortable, ipRGCs are leading suspects for contributing to photophobia.
However, additional studies from the same laboratory indicate rods and cones also contribute to photophobia. In dim lighting, when rods are active, retinas of people with migraines are more reactive to light than those without migraines. In addition, cones play a role in photophobia because people with migraines find blue, yellow, and red light painful but green light soothing and calming.
Light and pain converge in the posterior thalamus where some neurons respond to both forms of stimulation. In addition, direct connections from the eyes to the hypothalamus — the area of the brain regulating hunger, breathing rhythms, heart rate, and mood, among other things — may cause light to worsen symptoms, like nausea, rapid breathing, elevated heart rate, and negative emotions, in people with migraines.
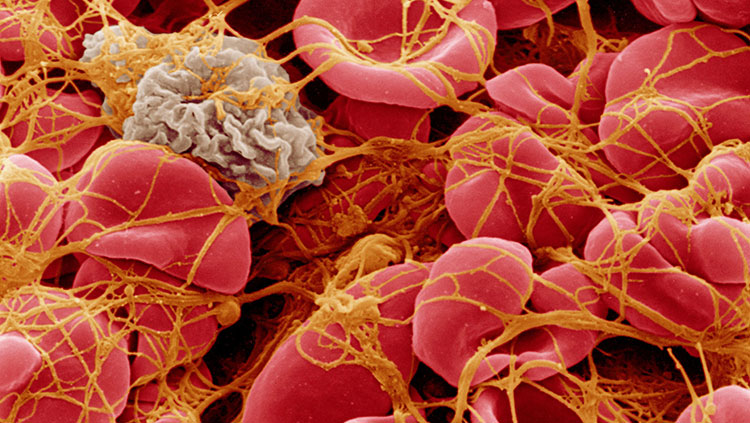
Pain-sensing nerves may also recruit the body’s inflammatory response to trigger pain and photophobia. Russo speculates that when blood vessels around the brain dilate, they can initiate positive feedback loops between trigeminal nerves and vessels. As a result, increased release of the peptide CGRP from pain-sensing nerves can further dilate vessels and activate immune cells. Since immune cells regulate the body’s inflammatory response, these series of events trigger migraine pain and photophobia. A study in mice demonstrated that CGRP opens blood vessels, and elevated levels of the protein in circulation drove the mice to scurry into the dark portion of their enclosures, reminiscent of photophobic behavior in humans.
People with migraines might be sensitive to triggers coming from both the outside world and their internal being. “Every person is exposed to these triggers, but only migraineurs develop pain which implies that the migraine brain is different,” Noseda says. “It’s more sensitive, it’s hyperexcitable.”
Understanding the underpinnings of photophobia may help prevent migraines. “We now know that light information from the retina can reach the hypothalamus and evoke different types of emotions, some of which can negatively affect the migraine experience,” Noseda says. “Therapies using green light at low intensities may help migraineurs feel better by evoking positive emotions.”
The prospect of simple solutions such as using green light to lessen photophobia is wildly encouraging to migraine sufferers. “Knowing that there is research out there that can used by people like me gives me hope that my migraines will be more manageable in the future,” Barger says. “I’m looking forward to it.”
CONTENT PROVIDED BY
BrainFacts/SfN
References
Bernstein, C. A., Nir, R.-R., Noseda, R., Fulton, A. B., Huntington, S., Lee, A. J., … Burstein, R. (2019). The migraine eye: distinct rod-driven retinal pathways’ response to dim light challenges the visual cortex hyperexcitability theory. PAIN, 160(3) 569–578. doi: 10.1097/j.pain.0000000000001434.
Kardon, R. (2012). Melanopsin and its role in photophobia. Acta Ophthalmologica, 90(s249), 0–0.
doi: 10.1111/j.1755-3768.2012.3865.x
Markwell, E. L., Feigl, B., & Zele, A. J. (2010). Intrinsically photosensitive melanopsin retinal ganglion cell contributions to the pupillary light reflex and circadian rhythm. Clinical and Experimental Optometry, 93(3), 137–149. doi: 10.1111/j.1444-0938.2010.00479.x
Mason, B. N., Kaiser, E. A., Kuburas, A., Loomis, M.-C. M., Latham, J. A., Garcia-Martinez, L. F., & Russo, A. F. (2017). Induction of Migraine-Like Photophobic Behavior in Mice by Both Peripheral and Central CGRP Mechanisms. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 37(1), 204–216. doi: 10.1523/JNEUROSCI.2967-16.2016
Noseda, R., Lee, A. J., Nir, R.-R., Bernstein, C. A., Kainz, V. M., Bertisch, S. M., … Burstein, R. (2017). Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proceedings of the National Academy of Sciences of the United States of America, 114(28), E5683–E5692.
doi: 10.1073/pnas.1708361114
Noseda, R., Bernstein, C. A., Nir, R.-R., Lee, A. J., Fulton, A. B., Bertisch, S. M., … Burstein, R. (2016). Migraine photophobia originating in cone-driven retinal pathways. Brain: A Journal of Neurology, 139(Pt 7), 1971–1986. doi: 10.1093/brain/aww119
Noseda, R., Kainz, V., Jakubowski, M., Gooley, J. J., Saper, C. B., Digre, K., & Burstein, R. (2010). A neural mechanism for exacerbation of headache by light. Nature Neuroscience, 13(2), 239–245.
doi: 10.1038/nn.2475