The Neuroscience of Touch and Pain
- Reviewed3 Feb 2020
- Author Sandra Blumenrath
- Source BrainFacts/SfN

When holding your friend’s hand, you feel the heat from their skin, the softness or roughness of their palm, and the pressure from their fingers. The sense of touch conveys important social information, helping strengthen bonds between people. If your friend grips your hand so hard it hurts, touch lets you know something is wrong or dangerous through the feeling of pain.
Cortical Maps and Sensitivity to Touch
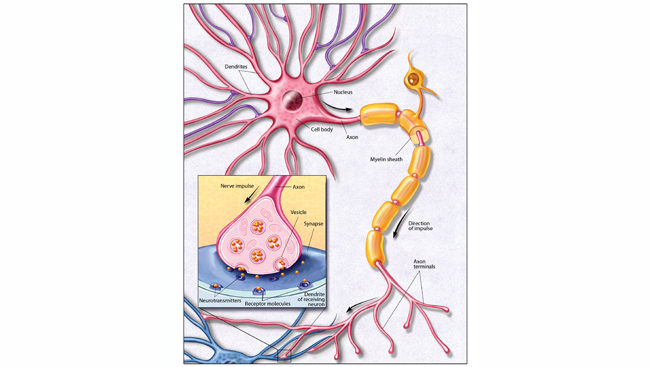
Sensations begin as signals generated by touch receptors in your skin. They travel along sensory nerves made up of bundled fibers that connect to neurons in the spinal cord. Then signals move to the thalamus, which relays information to the rest of the brain. Next stop is the somatosensory cortex, where signals are translated into a touch perception.
Somatosensory information from all over the body spreads onto the cortex forming a topographic map that curls around the brain like headphones. Sensitive areas, like lips and fingertips, stimulate much larger regions of the cortex than less sensitive parts. A region’s sensitivity depends on the number of receptors per unit area and the distance between them. Unlike the very sensitive lips and hands, receptors on your back are few and far apart so it’s much less sensitive.
Neurologists measure sensitivity by examining the minimum distance between two points on the skin a person can identify as distinct stimuli rather than a single stimulus. Perception is greatest where the two-point threshold is lowest, in the most densely nerve-packed areas, like fingers and lips. But you can distinguish two stimuli on your back only if they’re several centimeters apart.
Pain and Itch Signals
Stub your toe on a door jamb too hard and you’ll feel an uncomfortable sensation: pain. Primarily a warning signal, pain is the brain’s way of signaling something is wrong with the body. Both a sensory and emotional experience, pain signals tissue damage or the potential for damage and makes the experience feel unpleasant and upsetting.
After your toe encounters the door jamb, special sensory neurons, nociceptors, respond to the impact. Nociceptors are attuned to stimuli that cause tissue damage. They respond to strong stimuli, telling you when something is truly dangerous. Touching the door jamb gently isn’t harmful. Kick it too hard and you could break a bone. Different nociceptors are sensitive to different painful stimuli, like thermal (heat or cold), mechanical (wounds), and chemical (toxins or venoms).
Some nociceptors respond only to chemical stimuli causing itch. Histamine receptors activate when skin irritation, bug bites, or allergies trigger the release of histamine in the body. Itch receptors have molecular channels in their cell membrane that open when they detect histamine. Scientists have identified other itch-specific receptors that activate when they detect other molecules including, prostaglandins, neuropeptides, and proteases the body releases in response to pain and irritants.
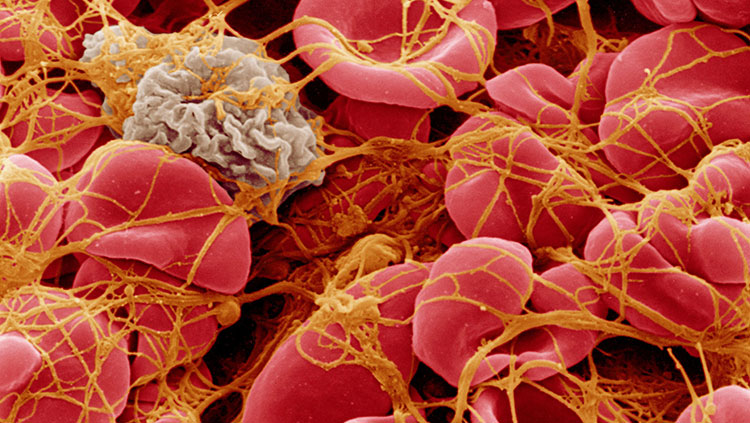
Injury triggers the release of various chemicals at the site of damage, causing inflammation. This inflammatory “soup” prompts nerve impulses that keep you feeling pain, so you’ll protect the injury. Prostaglandins make receptors more sensitive to pain, so pain feels more intense. A long-lasting injury may lead to nervous system changes that enhance perceived pain, even without pain stimuli. This neuropathic pain is caused by an over-sensitive nervous system rather than an injury. In diabetic neuropathy, prolonged exposure to high blood sugar damages nerves in the hands and feet, sending signals of numbness, tingling, burning, or aching pain.
Sending and Receiving Messages
Pain and itch messages travel to the spinal cord via A-delta and C nerve fibers. Myelinated A-delta fibers insulate the nerve, so electrons are channeled effectively and travel faster letting you feel immediate, sharp, and easily identifiable pain. Unmyelinated C fibers transmit messages more slowly and their nerve endings spread over a large area. They help you feel dull aches difficult to pinpoint. From the spinal cord, signals head to the thalamus, which relays signals to areas of the cerebral cortex transforming messages into conscious experience. Once aware, you can decide to be more careful the next time you approach the door.
Pain Management
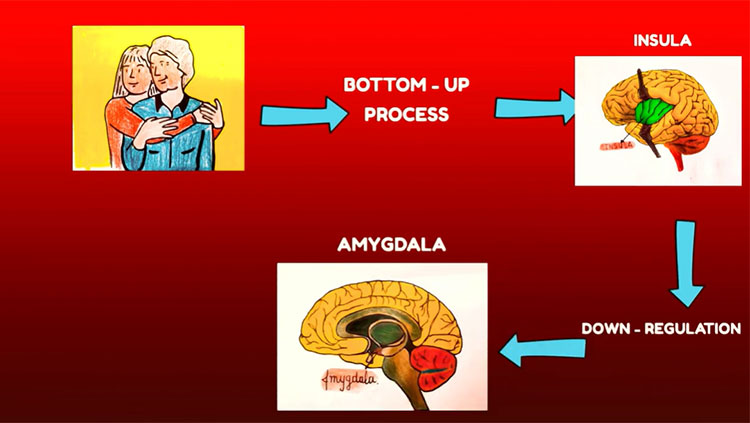
If you and your friend both stub the same toe on the same door jamb, you’ll probably experience the pain differently. Pain depends both on the strength of the stimulus and the emotional state and setting in which the injury occurs. When messages arrive in the cortex, the brain can process them differently depending on whether you had a good day or just broke up with your girlfriend.
The cortex sends pain messages to the periaqueductal gray matter, which activates pathways that modulate pain. Pathways send messages to networks that release endorphins — natural opioids that act like the pain reliever morphine. Adrenaline produced during emotionally stressful situations also serves as a pain reliever. Releasing these chemicals helps regulate and reduce pain by intercepting signals traveling through the spinal cord and brainstem.
Although everyone has these brain circuits, how well they work and how sensitive they are influence how much pain someone feels. It’s why some people develop chronic pain that regular treatment can’t relieve. Endorphins act at multiple types of opioid receptors in the brain and spinal cord. Doctors can deliver opioid drugs to the spinal cord before, during, and after surgery to reduce pain. Scientists are studying ways to electrically stimulate the spinal cord to relieve pain while avoiding the harmful effects of long-term opioid use.
No single brain area is responsible for pain and itch perception. Emotional and sensory components create a mosaic of activity influencing how we perceive pain. Some successful treatments target the emotional component like meditation, hypnosis, cognitive behavioral therapy, and the controlled use of cannabis. Patients with chronic pain still feel pain, but it doesn’t “hurt” as much. Brain imaging shows that cannabis suppresses activity in only a few pain areas, mostly the limbic system, the brain’s emotional center. Scientists don’t fully understand how these therapies work yet.
There is more to learn about how the brain and body detect and process touch and pain. The story so far shows the complexity and importance of the somatosensory system.
This article was adapted from the 8th edition of Brain Facts by Sandra Blumenrath.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Garibyan, L., Rheingold, C. G., & Lerner, E. A. (2013). Understanding the pathophysiology of itch. Dermatologic Therapy, 26(2), 84–91. doi: 10.1111/dth.12025