Snapshots into Traumatic Brain Injury
- Reviewed14 Aug 2023
- Author Gail Zyla
- Source BrainFacts/SfN

A big thump! to the head can do more than leave you seeing stars. It can have long-lasting impacts on your neurological function depending on the degree of injury.
*Traumatic brain injuries (TBIs) are caused by bumps, blows, or jolts to the head that cause multiple minuscule bleeds or penetrating head injuries that destroy brain tissue. These injuries may result in bruising of the brain's surface as it impacts the bony skull, stretching and shearing of brain cells, or tearing of blood vessels on or in the brain. In 2019, an estimated 223,000 people in the United States were hospitalized with traumatic brain injuries. CDC estimates report over 69,000 cases of TBI-related deaths in the U.S. in 2021 — around 190 TBI-related deaths every day. Falls are the leading cause of all traumatic brain injury, and firearm-related suicide is the leading cause of TBI-related death in the U.S. The direct medical costs and indirect costs of TBI, such as lost productivity, are estimated to be around $76.5 billion (in 2010 dollars) in the United States.
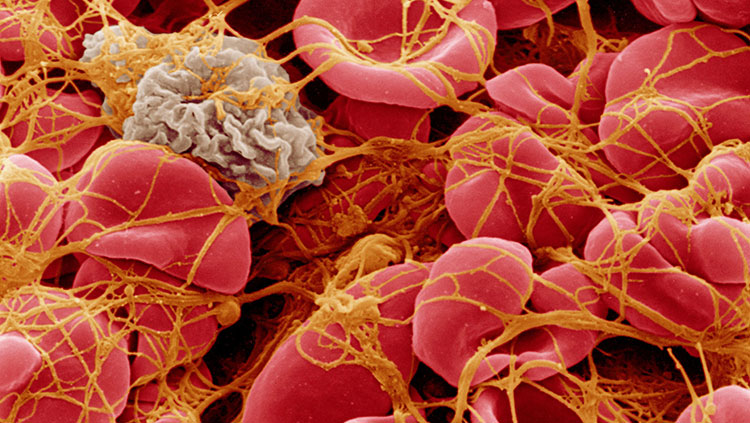
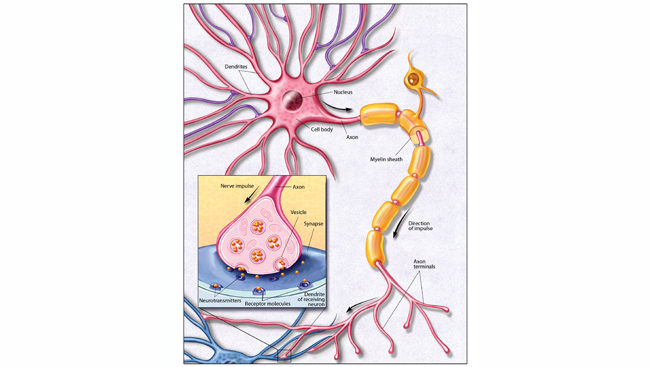
TBI can be “mild,” such as concussion — a temporary disruption in brain activity — or “severe,” such as an injury that leads to a prolonged period of unconsciousness. TBI can cause bruises to the surface of the brain, bleeding around the membranes covering the brain, cuts in brain tissue, and microscopic damage to axons, nerve cells, and blood vessels. Brain injury can trigger swelling, fever, seizures, and other neurological impairments. Even mild TBI can cause damage to neurons and other neural support cells, triggering the release of pro-inflammatory factors that initiate and sustain an inflammatory response. Widespread use of computerized tomography (CT) and magnetic resonance imaging (MRI) techniques has afforded opportunities to observe the extent of tissue damage in TBI and determine its medical management.
People such as professional football players or boxers, who sustain repeated concussions and other brain trauma, have a high risk of developing a progressive degenerative brain disease called chronic traumatic encephalopathy (CTE). CTE occurs when repeated head trauma triggers degeneration of brain tissue; this process includes a buildup of abnormal proteins, which can begin months, years, or even decades after the last brain trauma. Symptoms associated with CTE include memory loss, confusion, impaired judgment, impulse control problems, aggression, depression, and, eventually, progressive dementia.
Most people with mild brain injuries, such as concussions, recover fully in a short period of time — usually a few days to a few weeks. Yet a study of college ice hockey players who had concussions showed that their brain volume had decreased two weeks after the concussion, a change that lasted at least two months. Rest and avoiding physically demanding activities to give the brain time to heal are key aspects of recovery. People who arrive in the emergency department with a head injury are evaluated for brain bleeding or swelling, which may require a neurosurgical operation to decompress the skull and remove fluid from injured and inflamed brain tissue.
Severe TBIs can cause bruising on the surface or within the brain. The bruising might cause blood to leak from vessels directly onto brain tissue, which can be toxic to brain cells. Pressure often increases in the injured area, compresses the blood vessels, and reduces critical blood flow to the injured tissues. If fluid removal and medications fail to decrease pressure on the brain, part of the skull can be drilled open or removed to relieve pressure on the brain in the clinic. In some cases of TBI, bruising in the brain can contribute to the development of a seizure disorder called post-traumatic epilepsy.
Scientists have discovered that neurogenesis, the production and growth of new nerve cells, can occur in certain regions of the adult brain. However, these cells do not seem to help an injured brain repair itself, so studies are ongoing to determine how to jumpstart the pathway that stimulates the birth of new nerve cells. Some studies use stem cells, which can be influenced to produce many different cell types — nerve cells among them, to better understand brain cell growth and repair. Ongoing research aims to figure out how certain neurochemical and cellular barriers that prevent regrowth and repair can be overcome and how the newly born cells can be induced to integrate into the injured circuit.
Once a person with a brain injury is stable, the long road to recovery begins. Physical and occupational therapy are used to help people regain lost functions such as speech and movement. A wide variety of medications can be used to treat other symptoms of TBI such as pain, seizures, muscle spasms, sleep disorders, depression, and anxiety.
*This paragraph was updated August 14, 2023, to reflect the most recent CDC data for TBI prevalence.
If you or someone you know in the U.S. is struggling with self-harm or thoughts of suicide, visit or call the National Suicide Prevention Lifeline at 988 or 1-800-273-8255. The lifeline provides free and confidential support 24 hours a day, 7 days a week. If you or someone you know is in danger or needs immediate medical attention, please call 911 or visit your nearest emergency medical center.
Adapted from the 8th edition of Brain Facts by Gail Zyla.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Brain Tumor Society. (2023). Brain Tumor Facts. Brain Tumors. https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-facts/
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Cancer Institute. (2023). Brain Tumor. NCI Dictionary of Cancer Terms. NIH. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/brain-tumor
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false